About aprotinin
Aprotinin is indicated for prophylactic use to reduce blood loss and blood transfusion in adult patients at high risk of major blood loss undergoing isolated cardiopulmonary bypass graft surgery (i.e. coronary artery bypass graft surgery that is not combined with other cardiovascular surgery). Aprotinin should only be used after careful consideration of the benefits and risks, and alternative treatments.1
Aprotinin can reduce blood loss and the need for transfusion in appropriate patients undergoing isolated CABG1,2
Aprotinin is a serine protease inhibitor that has effects on coagulation, fibrinolysis, and platelet function.1,2
These mechanisms of action help mitigate tissue reperfusion injury and changes in the patient’s coagulation cascade and systemic inflammatory response, post isolated CABG.2
Aprotinin inhibits a number of serine proteases in the coagulation and fibrinolytic cascades.2
To find out more about the impact of Aprotinin on the coagulation and fibrinolytic cascades, hover your cursor over the information icons in the diagram below
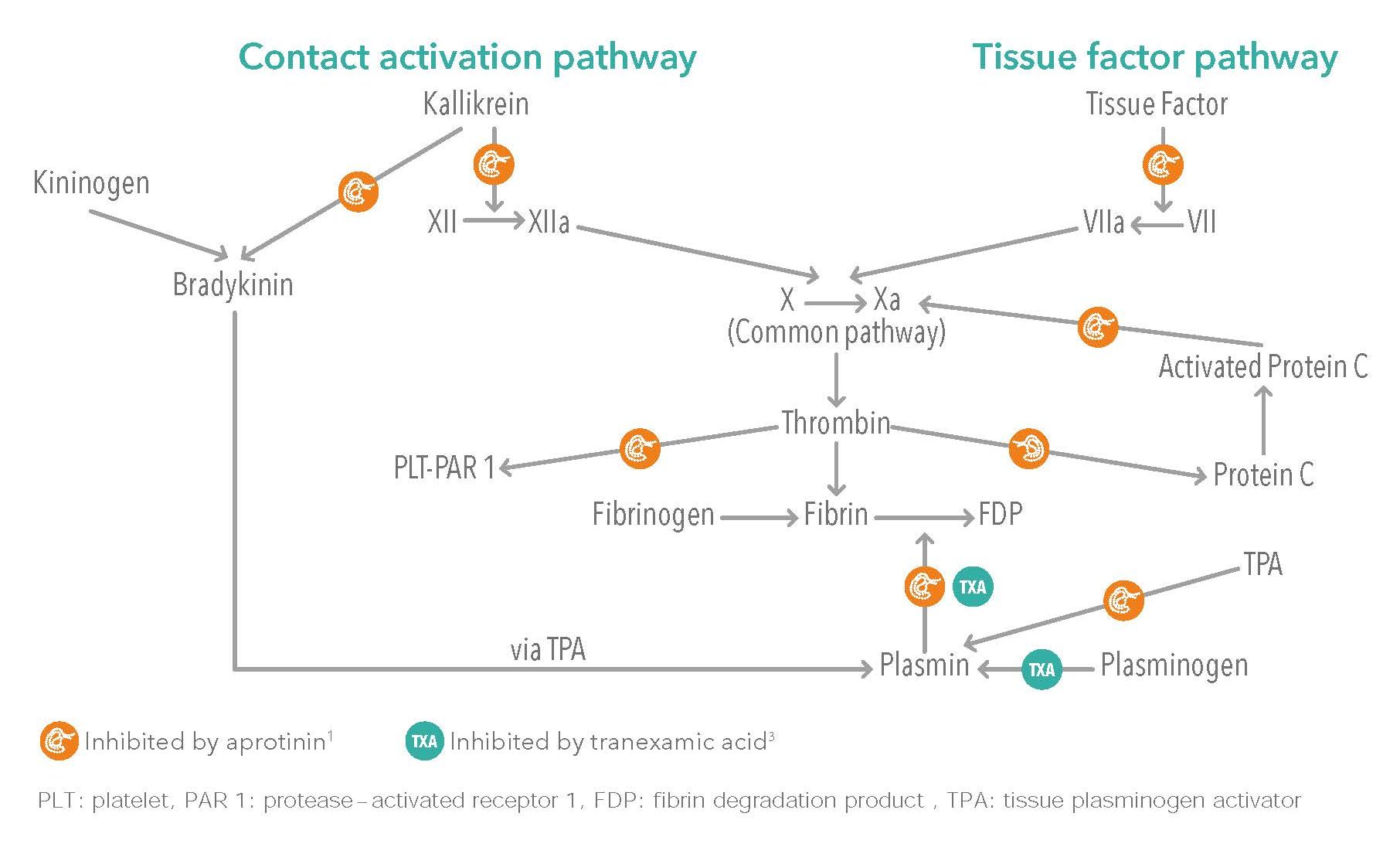
Adapted from McEvoy MD. et al.2
Aprotinin inhibits both the contact activation and tissue factor pathways helping to reduce the risk of bleeding.3
Understanding aprotinin safety4-9
In 2007, the company responsible for marketing aprotinin suspended the licence following the release of some preliminary data suggesting an increased mortality in aprotinin treated patients in the Blood Conservation Using Antifibrinolytics in a Randomized Trial (BART) trial, published in May 2008.4-6 The results from this study have since been questioned due to several methodological deficiencies.
The licence suspension for aprotinin was lifted in 2013, supported by additional data and new analyses.5-7
Full analysis of the BART dataset showed:7
- Aprotinin was associated with a lower risk of massive bleeding than either tranexamic or ε-aminocaproic acid
- Aprotinin was not associated with a significantly higher risk of stroke, myocardial infarction or renal failure/dysfunction compared with the other antifibrinolytics.
A meta-analysis that included the BART data further explored the safety profile of aprotinin, finding:7
- No difference in mortality between placebo and antifibrinolytic agents
- No difference in mortality between aprotinin and tranexamic acid (17 trials) or between aprotinin and ε-aminocaproic acid (six trials)
These findings are consistent with other reviews of aprotinin, which have observed:
- No increased risk of myocardial infarction, stroke, or renal dysfunction/failure vs. placebo8
- The benefits of aprotinin outweigh the associated risks in appropriate patients9
- A risk–benefit profile that led to the recommendation for lifting the aprotinin licence suspension5
Renal impairment: Renal dysfunction could be triggered by aprotinin, particularly in patients with pre-existing renal dysfunction. Careful consideration of the balance of the risks and benefits is therefore advised before administration of aprotinin to patients with pre-existing impaired renal function or those with risk factors (such as concomitant treatment with aminoglycosides).1
A transient rise in creatinine observed in some patients receiving aprotinin has been shown to normalise at post-operative day 3.10
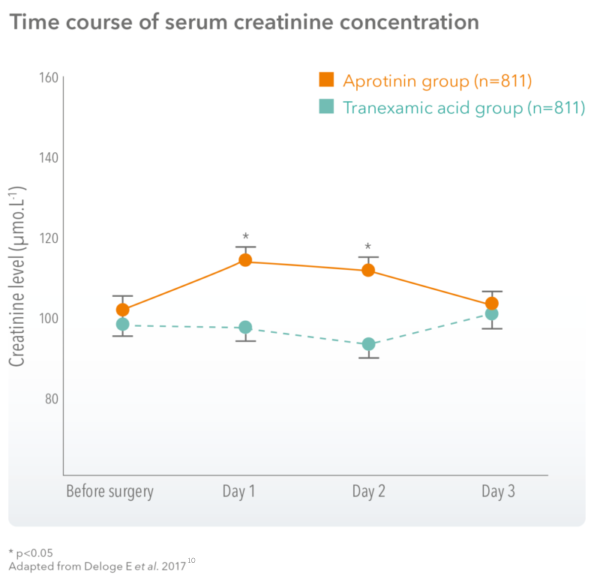
A transient rise in creatinine observed in patients receiving aprotinin resolves to normal levels by post-operative day 3, at which point there was no difference between treatment arms.10
References
-
- Aprotinin 10,000 KIU/ml Injection BP Summary of Product Characteristics. Available from: https://www.medicines.org.uk/emc/product/2472/smpc.
- McEvoy MD et al. Aprotinin in Cardiac Surgery: A Review of Conventional and Novel Mechanisms of Action. Anesth Analg. 2007;105:949–62.
- Tranexamic Acid 100mg/ml Solution for Injection Summary of Product Characteristics.
- European Society of Anaesthesiology task force reports on place of aprotinin in clinical anaesthesia. Aprotinin: Is It Time to Reconsider? Eur J Anaesthesiol. 2015;32:591–5.
- European Medicines Agency. Assessment report. Antifibrinolytics containing aprotinin, aminocaproic acid and tranexamic acid. 18 September 2013. Available from: https://www.ema.europa.eu/en/documents/referral/assessment-report-antifibrinolytic-medicines-aprotinin_en.pdf.
- Fergusson DA et al. A Comparison of Aprotinin and Lysine Analogues in High-Risk Cardiac
Surgery. N Engl J Med. 2008;358:2319–2331. - Howell N et al. J Thorac Cardiovasc Surg. 2013;145:234–40.
- Henry DA, et al. Anti-fibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 2011;(1):CD001886.
- Health Canada. Final report—expert advisory panel on Trasylol (aprotinin) 2011: Available from: https://healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2011/13544a-eng.php
- Deloge E et al. Aprotinin vs. tranexamic acid in isolated coronary artery bypass surgery. Eur J Anaesthesiol 2017;34:1–8.
