Which patients undergoing isolated CABG are at high risk of transfusion and what is the impact?
Blood loss and transfusions remain common in cardiac surgery1–3
Long-term studies have shown a consistently high requirement for transfusion during isolated coronary artery bypass grafting (CABG) procedures. Over half of patients undergoing an isolated CABG required some degree of transfusion, and 80% required at least two units of red blood cells (RBC).1
Despite the use of tranexamic acid, 30% (n=700/2342) of patients undergoing CABG required a major transfusion (4 or more RBC).2
Blood loss is relatively common in isolated CABG regardless of cardiopulmonary bypass support: meaningful blood loss (greater than 2L) is seen in 5–7% of patients, and 5% of patients require re-intervention for bleeding after sternotomy closure.3
Transfusions are associated with increased morbidity and mortality4,5
Blood transfusions are common in isolated CABG, and even transfusions of one or two units of RBC are associated with dose-dependent worsened outcomes and increasing risk of morbidity and mortality.1,4,5
Patients who received RBC transfusions have greater post-operative mortality than non-transfused patients.5
Aggressive attempts at blood conservation and avoidance of even small amounts of RBC transfusion may improve outcomes after isolated CABG.4
* Results of an observational cohort study of 11,963 patients who underwent isolated CABG at a tertiary care institution.
Adapted from Koch et al. 20065
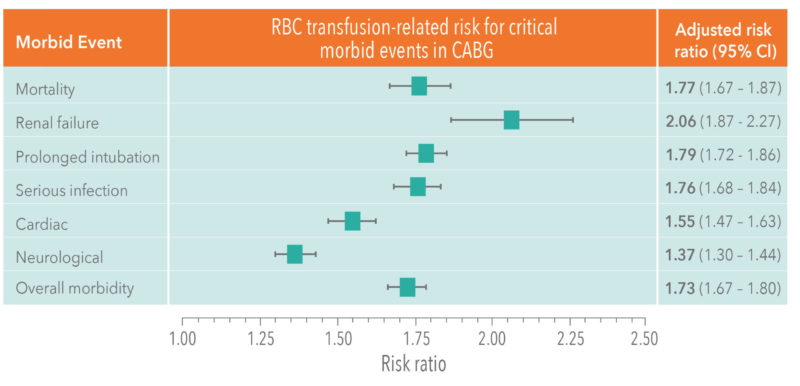
Red blood cell transfusions are associated with worsened outcomes and increasing risk of morbidity and mortality5
RBC transfusion presents a dose-dependent increase in risk of in-hospital mortality.5 Even one unit of RBC increases the risk of death by 77% (odds ratio [OR], 1.77; 95% confidence interval [CI], 1.67–1.87; p < .0001), compared with people who do not receive a transfusion – and this risk increases even more dramatically with transfusion of more than five units of RBC.5
Identifying patients who are most likely to require transfusion during cardiac surgery2
There are several significant independent risk factors that are predictive of requiring a major transfusion.
| Risk factors predictive of ICABG patients requiring major transfusion | |
|
|
Up to 40% of patients undergoing cardiac surgery have anaemia,6 which is associated with increased risk of requiring post-surgery blood transfusion.6,7
Patients with anaemia are also at risk of poorer outcomes, longer hospital stays and of increased mortality.7
It is therefore important to assess individual patient risk factors when considering the need for blood conservation methods. The definition of ‘high risk’ should be informed by the individual patient’s characteristics, rather than the complexity of surgery.8
To find out more about aprotinin
References
- Gombotz H et al. The second Austrian benchmark study for blood use in elective surgery: results and practice change. Transfusion 2014;54:2646–57.
- Stevens LM et al. Major transfusions remain frequent despite the generalized use of tranexamic acid: an audit of 3322 patients undergoing cardiac surgery. Transfusion 2016;56:1857–65.
- Mehran R et al. Standardized bleeding definitions for cardiovascular clinical trials. Circulation 2011;123:2736-2747.
- Paone G et al. Transfusion of 1 and 2 units of red blood cells is associated with increased morbidity and mortality. Ann Thorac Surg. 2014;97:87–94.
- Koch CG et al. Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med 2006;34:1608–1616.
- Boer C et al. 2017 EACTS/EACTA Guidelines on patient blood management for adult cardiac surgery. J Cardiothor Vasc Anesth. 2018;32:88–120.
- Klein AA et al. The incidence and importance of anaemia in patients undergoing cardiac surgery in the UK – the first Association of Cardiothoracic Anaesthetists national audit. Anaesthesia. 2016;71:627–35.
- European Society of Anaesthesiology task force reports on place of aprotinin in clinical anaesthesia. Aprotinin: Is It Time to Reconsider? Eur J Anaesthesiol. 2015;32:591–5.
